99231 : Inpatient hospital visits: Initial and subsequent
subsequent hospital care, per day, for the evaluation and management of a patient, which requires at least 2 of the 3 key components: A problem focused interval history; A problem focused examination; Medical decision making that is straightforward or of low complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is stable, recovering or improving. Physicians typically spend 15 minutes at the bedside and on the patient’s hospital floor or unit.
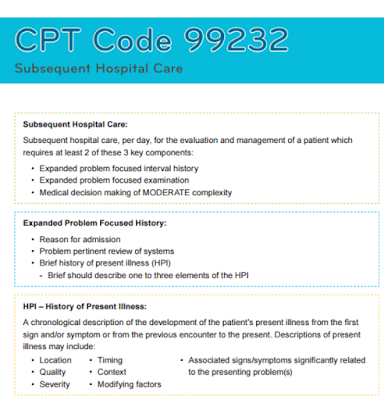
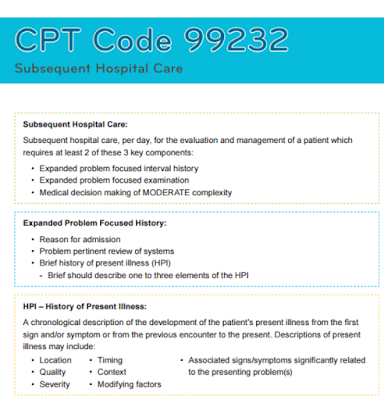
99232 : Inpatient hospital visits: Initial and subsequent
subsequent hospital care, per day, for the evaluation and management of a patient, which requires at least 2 of the 3 key components: An expanded problem focused interval history; An expanded problem focused examination; Medical decision making of moderate complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is responding inadequately to therapy or has developed a minor complication. Physicians typically spend 25 minutes at the bedside and on the patient’s hospital floor or unit.
99233 : Inpatient hospital visits: Initial and subsequent
subsequent hospital care, per day, for the evaluation and management of a patient, which requires at least 2 of the 3 key components: A detailed interval history; A detailed examination; Medical decision making of high complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is unstable or has developed a significant complication or a significant new problem. Physicians typically spend 35 minutes at the bedside and on the patient’s hospital floor or unit.
CPT codes 99231-99233 are used to describe subsequent hospital care. These codes require documentation of the interval history at either problem focused, expanded problem focused, or detailed levels. The examination requires the same levels of documentation. The Medical decision making documentation must support straightforward, low, moderate, or high complexity. The nature of the presenting problem usually determines the levels of history and physical exam required.
1. CPT code 99231 usually requires documentation to support that the patient is stable, recovering, or improving.
2. CPT code 99232 usually requires documentation to support that the patient is responding inadequately to therapy or has developed a minor complication. Such minor complications might include careful monitoring of co-morbid conditions requiring continuous active management
3. CPT code 99233 usually requires documentation to support that the patient is unstable or has a significant new problem or complication.
Reporting Initial Hospital Care Codes
CMS is aware of concerns pertaining to reporting initial hospital care codes for services that previously could have been reported with CPT consultation codes, for which the minimum key component work and/or medical necessity requirements for CPT codes 99221 through 99223 are not documented.
** Physicians may bill initial hospital care service codes (99221-99223), for services that were reported with CPT consultation codes (99241 – 99255) prior to January 1, 2010, when the furnished service and documentation meet the minimum key component work and/or medical necessity requirements. Physicians must meet all the requirements of the initial hospital care codes, including “a detailed or comprehensive history” and “a detailed or comprehensive examination” to report CPT code 99221, which are greater than the requirements for consultation codes 99251 and 99252.
** In situations where the minimum key component work and/or medical necessity requirements for initial hospital care services are not met, subsequent hospital care CPT codes (99231 and 99232) could potentially be reported for an E/M service that could be described by CPT consultation code 99251 or 99252.
** Subsequent hospital care CPT codes 99231 and 99232, respectively, require “a problem focused interval history” and “an expanded problem focused interval history.” An E/M service that could be described by CPT consultation code 99251 or 99252 could potentially meet the component work and medical necessity requirements to report 99231 or 99232. Physicians may report a subsequent hospital care CPT code for services that were reported as CPT consultation codes (99241 – 99255) prior to January 1, 2010, where the medical record appropriately demonstrates that the work and medical necessity requirements are met for reporting a subsequent hospital care code (under the level selected), even though the reported code is for the provider’s first E/M service to the inpatient during the hospital stay.
** Reporting CPT code 99499 (Unlisted evaluation and management service) should be limited to cases where there is no other specific E/M code payable by Medicare that describes that service. Reporting CPT code 99499 requires submission of medical records and contractor manual medical review of the service prior to payment. Contractors shall expect reporting under these
circumstances to be unusual.
Medicare contractors have been advised to expect changes to physician billing practices accordingly. Contractors will not find fault with providers who report subsequent hospital care codes (99231 and 99232) in cases where the medical record appropriately demonstrates that the work and medical necessity requirements are met for reporting a subsequent hospital care code (under the level selected) .
An important step in strengthening the links in your processes is to coordinate with other physicians, qualified health care professionals, and/or agencies. This will help ensure the counseling and/or care provided is consistent with the nature of the problems and the family’s needs. Be certain to review the record with these questions in mind:
1.Is the history problem focused, expanded problem focused or a detailed interval history ?
Remember that an interval history is one that documents an update on the patient from the last encounter.
2.Is the exam a focused exam, which is CPT code 99231; an expanded problem focused exam, code 99232; or a detailed exam, code 99233 ?
3.Is the medical decision making straight forward or low complexity, code 99231; moderate complexity, code 99232; or high complexity, which would be code 99233 ?
4. How much time did the physician spend at the patient’s bedside ? Time is a factor that indicates the extent of the illness.
This will guide you in selecting the correct CPT code. Some other helpful tips to decrease denials include:
** Submit records within the 30-day time frame when Additional Documentation letters are received.
** Review medical documentation prior to submission for correct patient name and date of service.
** Verify that the provider’s signature is legible, or that there a signature log on file with Palmetto GBA.
** Verify that the complete date of service is legibly noted on all documentation.
Evaluation & management tips: Subsequent hospital care
Key points to remember
The key components (elements of service) of evaluation & management (E/M) services are:
1. History,
2. Examination, and
3. Medical decision-making.
When billing subsequent hospital care, two of the three key components must be fully documented in order to bill. When counseling and/or coordination of care dominates (more than 50 percent) the physician/patient and/or family encounter (at the bedside and floor/unit time in the hospital), then time may be considered the key or controlling factor to qualify for a particular level of E/M services. The extent of such time must be documented in the medical record.
CPT codes and requirements
99231 – 15 minutes (average)
• Problem focused interval history.
• Chief complaint
• Brief history of present illness
• Problem focused examination. Documentation needed:
• Limited examination of the affected body area or organ system
• Medical decision making that is straightforward OR of low complexity. Documentation needed (two of three below must be met or exceeded):
• Straightforward – Minimal number of diagnoses or management options; None or minimal amount and/or complexity of data to be reviewed; Minimal risk of significant complications, morbidity and/or mortality
• Low Complexity – Limited number of diagnoses or management options; Limited amount and/or complexity of data to be reviewed; low risk of significant complications, morbidity and/or mortality
99232 – 25 minutes (average)
• Expanded problem focused interval history.
• Chief complaint
• Brief history of present illness
• Problem pertinent review of systems
• Expanded problem focused examination. Documentation needed:
• Limited examination of the affected body area or organ system and any other symptomatic or related body area(s)or organ system(s)
• Medical decision making that is moderate complexity. Documentation needed (two of three below must be met or exceeded):
• Multiple number of diagnoses or management options
• Moderate amount and/or complexity of data to be reviewed
• Moderate risk of significant complications, morbidity and/or mortality
99233 – 35 minutes (average)
• Detailed interval history.
• Chief complaint
• Extended history of present illness
• Extended review of systems
• Pertinent past, family and/or social history
• Detailed examination. Documentation needed:
• Extended examination of the affected body area(s) or organ system(s) and any other symptomatic or related body area(s) or organ system(s)
• Medical decision making that is of high complexity. Documentation needed (two of three below must be met or exceeded):
• Extensive number of diagnoses or management options
• Extensive amount and/or complexity of data to be reviewed
• High risk of significant complications, morbidity and/or mortality
Clinical Example:
Coding of the visits during a six-day hospitalization of an eighty year old patient with a presumptive diagnosis of pneumococcal pneumonia and low oxygen saturation.
First day after the day of admission: The patient continues tachypnic with low oxygen saturation, and febrile. The patient is receiving oxygen and broad-spectrum antibiotics awaiting cultures results. At present there is an inadequate response and condition would appear to support the levels of history and Physical exam required for CPT
code 99232.
Second day after the day of admission: Less tachypnea, still febrile, still receiving oxygen and broad spectrum –antibiotics. Culture results isolate no specific pathogen and current antibiotics are continued. A continued inadequate response would appear to support the levels of history and Physical exam required for CPT code 99232.
Third day after day of admission: Patient is afebrile, room air oxygen saturation is good. Patient is obviously improved. Current antibiotics continued intravenously for one more day. The patient is recovering and improving. Condition would appear to support the levels of history and Physical exam required for CPT code 99231.
Fourth day after the day of admission: Afebrile with good room air oxygen saturation. IV antibiotics are discontinued and patient started on oral antibiotics. The patient is recovering and improving. Condition would appear to support the levels of history and Physical exam required for CPT code 99231.
Fifth day after day of admission: Patient is discharged and the appropriate discharge code is billed.
Admission Visit Daily Visit Consultation
Time (min) Code Time (min) Code Time (min) Code
30 99221 15 99231 20 99251 50 99222 25 99232 40 99252 70 99223 35 99233 55 99253 80 99254 110 99255
In situations where the minimum key component work and/or medical necessity requirements for initial hospital care services are not met, subsequent hospital care CPT codes (99231 and 99232) could potentially meet requirements to be reported for an E/M service that could be described by CPT consultation code 99251 or 99252. Contractors shall expect changes to physician billing practices accordingly. Medicare contractors shall not find fault with providers who report a subsequent hospital care code (99231 and 99232) in cases where the medical record appropriately demonstrates that the work and medical necessity requirements are met for reporting a subsequent hospital care code (under the level selected), even though the reported code is for the provider’s first E/M service to the inpatient during the hospital stay.
Subsequent hospital care CPT codes 99231 and 99232, respectively, require “a problem focused interval history” and “an expanded problem focused interval history.” An E/M service that could be described by CPT consultation code 99251 or 99252 could potentially meet the component work and medical necessity requirements to report 99231 or 99232. Physicians may report a subsequent hospital care CPT code for services that were reported as CPT consultation codes (99241 – 99255) prior to January 1, 2010, where the medical record appropriately demonstrates that the work and medical necessity requirements are met for reporting a subsequent hospital care code (under the level selected), even though the reported code is for the provider’s first E/M service to the inpatient during the hospital stay.
Chief Complaint:
The Chief Complaint is a concise statement from the patient describing:
• The symptom
• Problem
• Condition
• Diagnosis
• Physician recommended return, or other factor
that is the reason for the encounter
Review of Systems:
An inventory of body systems obtained through a series of questions
seeking to identify signs and/or symptoms which the patient may be experiencing or has
experienced.
For purpose of Review of Systems the following systems are recognized:
• Constitutional
(i.e., fever, weight loss)
• Eyes
• Ears, Nose, Mouth Throat
• Cardiovascular
• Respiratory
• Gastrointestinal
• Genitourinary
• Musculoskeletal
• Integumentary
(skin and/or breast)
• Neurologic
• Psychiatric
• Endocrine
• Hematologic/Lymphatic
• Allergic/Immunologic
Billing and Coding Guidelines.
Palmetto GBA focused on the Subsequent Hospital Care procedure range of 99231 through 99233.
When any level of subsequent hospital care is under review, the medical record should include results of diagnostic studies and changes to the patient’s status since the last assessment. Changes include history, physical condition and response to management.
An important step in strengthening the links in your processes is to coordinate with other physicians, qualified health care professionals, and/or agencies. This will help ensure the counseling and/or care provided is consistent with the nature of the problems and the family’s needs. Be certain to review the record with these questions in mind:
1. Is the history problem focused, expanded problem focused or a detailed interval history? Remember that an interval history is one that documents an update on the patient from the last encounter.
2. Is the exam a focused exam, which is CPT code 99231; an expanded problem focused exam, code 99232; or a detailed exam, code 99233?
3. Is the medical decision making straight forward or low complexity, code 99231; moderate complexity, code 99232; or high complexity, which would be code 99233?
4. How much time did the physician spend at the patient’s bedside? Time is a factor that indicates the extent of the illness. This will guide you in selecting the correct CPT code.
(Common Procedural Terminology (CPT) codes 99231, 99232, and 99233); and
30 days (CPT codes 99307, 99308, 99309, and 99310).
Definition – Hospital , hospital admission, Inpatient hospital expense
Hospital means a short-term acute care facility which:
1. Is duly licensed as a Hospital by the state in which it is located and meets the standards established for such licensing, and is either accredited by the Joint Commission on Accreditation of Healthcare Organizations or is certified as a Hospital provider under Medicare;
2. Is primarily engaged in providing inpatient diagnostic and therapeutic services for the diagnosis, treatment, and care of injured and sick persons by or under the supervision of Physicians or Behavioral Health Practitioners for compensation from its patients;
3. Has organized departments of medicine and major surgery, either on its premises or in facilities available to the Hospital on a contractual prearranged basis, and maintains clinical records on all patients;
4. Provides 24-hour nursing services by or under the supervision of a Registered Nurse;
5. Has in effect a Hospital Utilization Review Plan; and
6. Is not, other than incidentally, a Skilled Nursing Facility, nursing home, Custodial Care home, health resort, spa or sanitarium, place for rest, place for the aged, place for the treatment of Chemical Dependency, Hospice, or place for the provision of rehabilitative care.
Hospital Admission means the period between the time of a Participant’s entry into a Hospital or a Chemical Dependency Treatment Center as a Bed patient and the time of discontinuance of bed-patient care or discharge by the admitting Physician, Behavioral Health Practitioner or Professional Other Provider, whichever first occurs. The day of entry, but not the day of discharge or departure, shall be considered in determining the length of a Hospital Admission. If a Participant is admitted to and discharged from a Hospital within a 24-hour period but is confined as a Bed patient in a bed accommodation during the period of time he is confined in the Hospital, the admission shall be considered a Hospital Admission by BCBSTX.
Inpatient Hospital Expense means the Allowable Amount incurred for the Medically Necessary items of service or supply listed below for the care of a Participant, provided that such items are:
1. Furnished at the direction or prescription of a Physician, Behavioral Health Practitioner or Professional Other Provider; and
2. Provided by a Hospital or a Chemical Dependency Treatment Center; and
3. Furnished to and used by the Participant during an inpatient Hospital Admission.
An expense shall be deemed to have been incurred on the date of provision of the service for which the charge is made.
Inpatient Hospital Expense shall include:
1. Room accommodation charges. If the Participant is in a private room, the amount of the room charge in excess of the Hospital’s average semiprivate room charge is not an Eligible Expense.
2. All other usual Hospital services, including drugs and medications, which are Medically Necessary and consistent with the condition of the Participant. Personal items are not an Eligible Expense.
Medically Necessary Mental Health Care or treatment of Serious Mental Illness or treatment of Serious Mental Illness in a Psychiatric Day Treatment Facility, a Crisis Stabilization Unit or Facility, or a Residential Treatment Center for Children and Adolescents, in lieu of hospitalization, shall be Inpatient Hospital Expense.
Late Enrollee means any Employee or Dependent eligible for enrollment who requests enrollment in an Employer’s Health Benefit Plan (1) after the expiration of the initial enrollment period established under the terms of the first plan for which that Participant was eligible through the Employer, (2) after the expiration of an Open Enrollment Period, or (3) after the expiration of a special enrollment period.
Medicare Review on CPT 99232 AND 99233
The top services for First Coast Service Options Inc. (First Coast) with payment errors identified by Part B comprehensive error rate testing (CERT) continue to be evaluation and management services. First Coast conducted a data analysis for Current Procedural Terminology® (CPT®) codes 99232 and 99233 (subsequent hospital care). The data indicates specialties internal medicine and cardiology are the primary contributors to the CERT error rate for subsequent hospital care services. Documentation requirements the American Medical Association (AMA) CPT® manual defines code 99232 as follows: Subsequent hospital care, per day, for the evaluation and management of a patient, which requires at least 2 of these 3 key components:
*** An expanded problem focused interval history ;
*** An expanded problem focused examination;
*** Medical decision making of moderate complexity Counseling and/or coordination of care with other physicians, other qualified health care professionals, or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family needs. Usually, the patient is responding inadequately to therapy or has developed a minor complication. Typically, 25 minutes are spent at the bedside and on the patient’s hospital floor or unit.
The AMA CPT® manual defines code 99233 as follows: Subsequent hospital care, per day, for the evaluation and management of a patient, which requires at least two of
these three key components:
*** A detailed interval history ;
*** A detailed examination;
*** Medical decision making of high complexity Counseling and/or coordination of care with other physicians, other qualified health care professionals, or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family needs. Usually, the patient is unstable or has developed a significant new problem. Typically, 35 minutes are spent at the bedside and on the patient’s hospital floor or unit. First Coast and the Centers for Medicare & Medicaid Service (CMS) offer multiple resources addressing the documentation guidelines for E/M service levels at:
*** First Coast’s Evaluation and Management (E/M) services page, offering links to tools, FAQs, online learning, and additional resources.
*** CMS Internet-only manual (IOM) guidelines addressing multiple types and settings pertaining to E/M services.
First Coast actions
In response to the high percentage of error rates and the continual risks of improper payments associated with subsequent hospital care billed by internal medicine and cardiology specialists, First Coast will be implementing a prepayment medical review audit for CPT® codes 99232 and 99233 billed by cardiology; and CPT® codes 99232 billed by internal medicine specialty. The new audit will be based on a threshold of claims submitted for payment by cardiology and internal medicine specialties in an effort to reduce the error rates for these hospital services. The audit will be implemented for claims processed on or after March 15, 2016.
Readmission within 15 days to the Same Hospital (Unrelated Readmission)
If a beneficiary is readmitted to the same hospital within 15 days for a condition(s) unrelated to the previous admission (e.g., gall bladder removal, injuries due to a car accident), Medicaid considers the case a new admission for payment purposes.
** The provider must submit two separate claims to assure appropriate processing.
** A claim for the first admission must be submitted and paid prior to submission of the readmission claim.
** When completing the second (readmission) claim, the hospital must indicate the PACER number in the treatment authorization field and Occurrence Span Code 71 with “from” and “through” dates from the previous admission.
Readmission within 15 days to the Same Hospital (Related Admission)
If a beneficiary is readmitted to the same hospital within 15 days for a related (required as a consequence of the original admission) condition, Medicaid considers the admission and the related readmission as one episode for payment purposes. The
related admissions must be combined on a single claim. No PACER number is issued for continuation of care.
** Revenue code 0180 is used for the days the beneficiary was not in the hospital.
** Enter the number of leave days in the service units field.
** Leave the rate and total charges blank.
** Include the leave day units in the total units field.
** Report Occurrence Span Code 74 with “from” and “through” dates of the leave of absence.
** If the original admission has been submitted and paid, a replacement claim must be submitted that contains the combined services for the original admission and the readmission.
Readmission within 15 days to a Different Hospital
Enter the PACER number in the treatment authorization field and Occurrence Span Code 71 with “from” and “through” dates from the previous admission.
Transfers Authorization for a transfer is granted only if the transfer is medically necessary and the care/treatment is not available at the transferring hospital. Transfer for convenience is not considered. Authorization should be obtained by the next business day for emergent/urgent transfers.
** The receiving hospital enters the PACER number of the approved transfer in the treatment authorization field.
** Submission of documentation with the claim is not required when billing transfers.
Q: How do I bill my claims when a patient revokes or elects hospice coverage during his/her inpatient stay?
A: Electing or revoking the Medicare hospice benefit is the beneficiary’s choice. The patient or his/her representative may elect or revoke Medicare hospice care at any time in writing. The hospice cannot revoke the beneficiary’s election, nor request or demand that the patient revoke his/her election. If the patient revokes his/her hospice election, Medicare coverage of all benefits waived when hospice care was initially elected resumes under the traditional Medicare program. The information below provides a general guidance on how to submit claims.
When a beneficiary elects hospice during an inpatient stay:
• Bill traditional Medicare for period before hospice election
• Patient status code is 51 (discharge to hospice medical facility)
• Discharge date is the effective date of hospice election
• Bill hospice for period of care after hospice election
When a patient revokes hospice during an inpatient stay:
• Bill hospice for period up to hospice revocation
• Bill traditional Medicare for period after hospice revocation
• Admission date is same as the hospice revocation date
• Statement from date is the same as the hospice revocation date
Consultation Services versus hospital care codes
Effective January 1, 2010, the consultation codes are no longer recognized for Medicare Part Bpayment. Physicians shall code patient evaluation and management visits with E/M codes that represent where the visit occurs and that identify the complexity of the visit performed.
In the inpatient hospital setting and the nursing facility setting, physicians (and qualified nonphysician practitioners where permitted) may bill the most appropriate initial hospital care code (99221-99223), subsequent hospital care code (99231 and 99232), initial nursing facility care code (99304-99306), or subsequent nursing facility care code (99307-99310) that reflects the services the physician or practitioner furnished. Subsequent hospital care codes could potentially meet the component work and medical necessity requirements to be reported for an E/M service that could be described by CPT consultation code 99251 or 99252.
Contractors shall not find fault in cases where the medical record appropriately demonstrates that the work and medical necessity requirements are met for reporting a subsequent hospital care code (under the level selected), even though the reported code is for the provider’s first E/M service to the inpatient during the hospital stay. Unlisted evaluation and management service (code 99499) shall only be reported for consultation services when an E/M service that could be described by codes 99251 or 99252 is furnished, and there is no other specific E/M code payable by Medicare that describes that service. Reporting code 99499 requires submission of medical records and contractor manual medical review of the service prior to payment. CMS expects reporting under these circumstances to be unusual. T he principal physician of record is identified in Medicare as the physician who oversees the patient’s care from other physicians who may be furnishing specialty care. The principal physician of record shall append modifier “- AI” (Principal Physician of Record), in addition to the E/M code. Follow-up visits in the facility setting shall be billed as subsequent hospital care visits and subsequent nursing facility care visits.
In the CAH setting, those CAHs that use method II shall bill the appropriate new or established visit code for those physician and non-physician practitioners who have reassigned their billing rights, depending on the relationship status between the physician and patient.
In the office or other outpatient setting where an evaluation is performed, physicians and qualified nonphysician practitioners shall use the CPT codes (99201 – 99215) depending on the complexity of the visit and whether the patient is a new or established patient to that physician. All physicians and qualified nonphysician practitioners shall follow the E/M documentation guidelines for all E/M services. These rules are applicable for Medicare secondary payer claims as well as for claims in which Medicare is the primary payer
SERVICES INCLUDED IN THE INPATIENT PAYMENT
The following services are included in the inpatient payment:
* All routine services (e.g., room and board, nursing).
* All diagnostic/ancillary services (e.g., radiology, pharmacy, therapists, supplies, pathology).
* While a patient is in the inpatient setting, the facility charges for any services performed by persons or entities other than the patient’s hospital (e.g., an independent lab, a second hospital where no transfer occurs) are covered in the payment to the patient’s hospital and must not be billed separately. All charges must be included on the inpatient claim of the patient’s hospital.
Any payments due to the second party are the responsibility of the patient’s hospital.
* All pathology services that are performed by the pathologist but do not directly relate to the specific patient’s care.
* All emergency room services provided by the hospital that result in an inpatient admission to that hospital. All charges must be included on the inpatient claim.
* An orthosis or prosthesis that is required for inpatient treatment, a surgical postoperative procedure or as a routine service of the hospital should be included as a supply on the inpatient claim and is reimbursed under the appropriate DRG.
Examples of items that are included in the inpatient payment are:
* Pacemakers
* Hip replacements
* Made-to-measure braces for compression fractures
* Compression stockings (TED, Jobst)
* Halos
* Immediate post-surgical or early fitting of prosthetic devices, etc.
SERVICES EXCLUDED FROM THE INPATIENT PAYMENT
The following services are excluded in the inpatient payment:
* An orthosis or prosthesis that is required for rehabilitation and will be utilized after discharge, and/or is required to address a long term, lifetime, permanent need. An orthotist/prosthetist must bill these items separately to Medicaid. Prior authorization (PA) must first be obtained for appropriate procedure codes.
* Except as noted above, outpatient services may not be separately billed while a beneficiary is in the inpatient setting. All charges must be included on the inpatient claim.
* Any services that are covered by Medicaid and excluded from the inpatient payment may be separately billed if the provider of the service is properly enrolled in the program and a claim is submitted appropriately.
The following are examples of services excluded from the inpatient payment. This list may not be allinclusive:
* Anatomic pathology services provided directly by a pathologist.
* Orthoses/prostheses required for rehabilitation that will be utilized after discharge, and/or are required to address a long term, lifetime, permanent need. Additional examples of items that are excluded from the inpatient payment are a knee-ankle-foot orthosis or an ankle-foot orthosis.
* Professional services (e.g., practitioner, dental, podiatric, optometric).
* Services provided by a certified nurse midwife (CNM).
* Services provided by a certified registered nurse anesthetist (CRNA).
* Ambulance services.
Payment for Initial Hospital Care Services and Observation or Inpatient Care Services (Including Admission and Discharge Services)
A.Initial Hospital Care From Emergency Room
Contractors pay for an initial hospital care service if a physician sees a patient in the emergency room and decides to admit the person to the hospital. They do not pay for both E/M services. Also, they do not pay for an emergency department visit by the same physician on the same date of service. When the patient is admitted to the hospital via another site of service (e.g., hospital emergency department, physician’s office, nursing facility), all services provided by the physician in conjunction with that admission are considered part of the initial hospital care when performed on the same date as the admission.
B.Initial Hospital Care on Day Following Visit
Contractors pay both visits if a patient is seen in the office on one date and admitted to the hospital on the next date, even if fewer than 24 hours has elapsed between the visit and the admission.
C.Initial Hospital Care and Discharge on Same Day
When the patient is admitted to inpatient hospital care for less than 8 hours on the same date, then Initial Hospital Care, from CPT code range 99221 – 99223, shall be reported by the physician. The Hospital Discharge Day Management service, CPT codes 99238 or 99239, shall not be reported for this scenario.
When a patient is admitted to inpatient initial hospital care and then discharged on a different calendar date, the physician shall report an Initial Hospital Care from CPT code range 99221 – 99223 and a Hospital Discharge Day Management service, CPT code 99238 or 99239.
When a patient has been admitted to inpatient hospital care for a minimum of 8 hours but less than 24 hours and discharged on the same calendar date, Observation or Inpatient
Hospital Care Services (Including Admission and Discharge Services), from CPT code range 99234 – 99236, shall be reported.
D.Documentation Requirements for Billing Observation or Inpatient Care Services (Including Admission and Discharge Services)
The physician shall satisfy the E/M documentation guidelines for admission to and discharge from inpatient observation or hospital care. In addition to meeting the documentation requirements for history, examination and medical decision making documentation in the medical record shall include:
*Documentation stating the stay for hospital treatment or observation care status involves 8 hours but less than 24 hours;
*Documentation identifying the billing physician was present and personally performed the services; and
*Documentation identifying the admission and discharge notes were written by the billing physician.
E.Physician Services Involving Transfer From One Hospital to Another; Transfer Within Facility to Prospective Payment System (PPS) Exempt Unit of Hospital; Transfer From One Facility to Another Separate Entity Under Same Ownership and/or Part of Same Complex; or Transfer From One Department to Another Within Single Facility
Physicians may bill both the hospital discharge management code and an initial hospital care code when the discharge and admission do not occur on the same day if the transfer is between:
*Different hospitals;
*Different facilities under common ownership which do not have merged records; or
*Between the acute care hospital and a PPS exempt unit within the same hospital when there are no merged records.
In all other transfer circumstances, the physician should bill only the appropriate level of subsequent hospital care for the date of transfer.
F.Initial Hospital Care Service History and Physical That Is Less Than Comprehensive
When a physician performs a visit that meets the definition of a Level 5 office visit several days prior to an admission and on the day of admission performs less than a
comprehensive history and physical, he or she should report the office visit that reflects the services furnished and also report the lowest level initial hospital care code (i.e., code 99221) for the initial hospital admission. Contractors pay the office visit as billed and the Level 1 initial hospital care code.
Physicians who provide an initial visit to a patient during inpatient hospital care that meets the minimum key component work and/or medical necessity requirements shall report an initial hospital care code (99221-99223). The principal physician of record shall append modifier “-AI” (Principal Physician of Record) to the claim for the initial hospital care code. This modifier will identify the physician who oversees the patient’s care from all other physicians who may be furnishing specialty care.
Physicians may bill initial hospital care service codes (99221-99223), for services that were reported with CPT consultation codes (99241 – 99255) prior to January 1, 2010, when the furnished service and documentation meet the minimum key component work and/or medical necessity requirements. Physicians must meet all the requirements of the initial hospital care codes, including “a detailed or comprehensive history” and “a detailed or comprehensive examination” to report CPT code 99221, which are greater than the requirements for consultation codes 99251 and 99252.
Subsequent hospital care CPT codes 99231 and 99232, respectively, require “a problem focused interval history” and “an expanded problem focused interval history.” An E/M service that could be described by CPT consultation code 99251 or 99252 could potentially meet the component work and medical necessity requirements to report 99231 or 99232. Physicians may report a subsequent hospital care CPT code for services that were reported as CPT consultation codes (99241 – 99255) prior to January 1, 2010, where the medical record appropriately demonstrates that the work and medical necessity requirements are met for reporting a subsequent hospital care code (under the level selected), even though the reported code is for the provider’s first E/M service to the inpatient during the hospital stay.
Reporting CPT code 99499 (Unlisted evaluation and management service) should be limited to cases where there is no other specific E/M code payable by Medicare that describes that service. Reporting CPT code 99499 requires submission of medical records and contractor manual medical review of the service prior to payment.
Contractors shall expect reporting under these circumstances to be unusual.
G.Initial Hospital Care Visits by Two Different M.D.s or D.O.s When They Are Involved in Same Admission
In the inpatient hospital setting all physicians (and qualified nonphysician practitioners where permitted) who perform an initial evaluation may bill the initial hospital care codes (99221 – 99223) or nursing facility care codes (99304 – 99306). Contractors consider only one M.D. or D.O. to be the principal physician of record (sometimes referred to as the admitting physician.) The principal physician of record is identified in Medicare as the physician who oversees the patient’s care from other physicians who may be
furnishing specialty care. Only the principal physician of record shall append modifier “- AI” (Principal Physician of Record) in addition to the E/M code. Follow-up visits in the facility setting shall be billed as subsequent hospital care visits and subsequent nursing facility care visits.